Laparoscopy, Hysteroscopy, and Ovarian Drilling: Advancing Infertility Care
Add to
Share
2,019 views
Report
2 years ago
Description
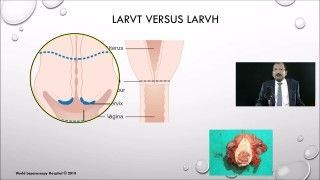
Introduction: Infertility is a distressing condition that affects numerous couples worldwide. In the quest to overcome infertility, medical advancements have led to the development of diagnostic laparoscopy and hysteroscopy with ovarian drilling, offering a comprehensive approach to infertility evaluation and treatment. This essay explores how these procedures have revolutionized the field, providing valuable insights into the causes of infertility and enabling targeted interventions to improve the chances of successful conception. Diagnostic Advancements: Diagnostic laparoscopy and hysteroscopy play a crucial role in identifying the underlying causes of infertility. Laparoscopy involves the insertion of a small camera through a tiny incision in the abdomen, allowing visualization of the pelvic organs. This technique provides a detailed view of the reproductive organs, enabling the detection of conditions such as endometriosis, tubal blockages, and uterine abnormalities. Similarly, hysteroscopy involves the insertion of a thin, lighted telescope into the uterus to examine its inner lining. This procedure helps identify issues such as uterine polyps, fibroids, and abnormalities in the shape or structure of the uterus. By accurately diagnosing these underlying conditions, laparoscopy and hysteroscopy guide the subsequent treatment approach, leading to more targeted and effective interventions. Ovarian Drilling for Polycystic Ovary Syndrome: In cases of infertility associated with polycystic ovary syndrome (PCOS), ovarian drilling is a valuable therapeutic option. This procedure, often performed during laparoscopy, involves puncturing the ovarian follicles using heat or laser to stimulate ovulation. By reducing the number of ovarian follicles and restoring hormonal balance, ovarian drilling improves the chances of successful ovulation and subsequent pregnancy. It offers an alternative to medications like clomiphene citrate or gonadotropins, particularly in cases where these medications have not yielded the desired results. Benefits of Minimally Invasive Surgery: Both laparoscopy and hysteroscopy are minimally invasive procedures, offering several advantages over traditional open surgery. With smaller incisions, patients experience reduced postoperative pain, minimal scarring, and shorter recovery times. Minimally invasive surgery also decreases the risk of complications, allowing individuals to resume normal activities sooner and increasing their overall satisfaction with the treatment process. These benefits contribute to enhanced patient well-being and quality of life throughout their infertility journey. Tailored Treatment Approach: The combined approach of diagnostic laparoscopy and hysteroscopy with ovarian drilling allows for a personalized treatment plan based on the specific underlying causes of infertility. By identifying and addressing factors such as endometriosis, tubal blockages, uterine abnormalities, or PCOS, clinicians can tailor interventions to each individual's unique needs. This targeted approach increases the likelihood of successful conception and improves the overall reproductive outcomes for couples struggling with infertility. This topic explores the advancements in infertility evaluation and treatment through the use of diagnostic laparoscopy and hysteroscopy with ovarian drilling. Infertility is a challenging condition that affects many couples worldwide, and these procedures have revolutionized the field by providing a comprehensive approach to understanding and addressing infertility. The essay highlights how diagnostic laparoscopy and hysteroscopy play a vital role in identifying the underlying causes of infertility. Laparoscopy allows for a visual examination of the pelvic organs, aiding in the detection of conditions such as endometriosis, tubal blockages, and uterine abnormalities. Similarly, hysteroscopy provides insights into the inner lining of the uterus, helping to identify issues like polyps, fibroids, or structural abnormalities. By accurately diagnosing these conditions, these procedures guide subsequent treatment plans, leading to more targeted and effective interventions. Furthermore, the essay emphasizes the use of ovarian drilling, particularly in cases of infertility associated with polycystic ovary syndrome (PCOS). Ovarian drilling, performed during laparoscopy, involves puncturing the ovarian follicles to stimulate ovulation. This procedure aims to reduce the number of ovarian follicles and restore hormonal balance, enhancing the chances of successful ovulation and subsequent pregnancy. The description highlights the benefits of minimally invasive surgery in these procedures. With smaller incisions, patients experience reduced postoperative pain, minimal scarring, and shorter recovery times. This less invasive approach also decreases the risk of complications and allows individuals to resume their normal activities sooner, improving their overall experience and well-being. The essay concludes by emphasizing the personalized and tailored treatment approach made possible by diagnostic laparoscopy and hysteroscopy with ovarian drilling. By identifying and addressing specific underlying causes, healthcare professionals can provide targeted interventions that increase the likelihood of successful conception and improve reproductive outcomes for couples struggling with infertility. Overall, the description showcases how diagnostic laparoscopy and hysteroscopy with ovarian drilling have transformed the field of infertility evaluation and treatment. It highlights the importance of accurate diagnosis, the benefits of minimally invasive surgery, and the personalized approach to care, offering hope and support to couples seeking to overcome infertility challenges. Conclusion: Diagnostic laparoscopy and hysteroscopy with ovarian drilling have revolutionized the evaluation and treatment of infertility. These procedures provide valuable insights into the underlying causes of infertility, enabling clinicians to tailor interventions and improve the chances of successful conception. With their minimally invasive nature, laparoscopy and hysteroscopy offer multiple benefits, including reduced postoperative pain, faster recovery, and decreased risk of complications. By embracing these advancements, healthcare professionals can provide more effective and personalized care, offering hope and support to couples on their infertility journey.
Similar Videos