Stepwise Laparoscopic Sigmoidectomy with Total Mesorectal Excision
Add to
Share
22 views
Report
2 days ago
Description
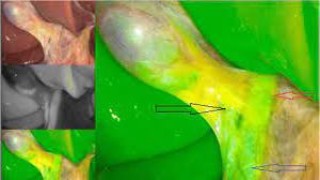
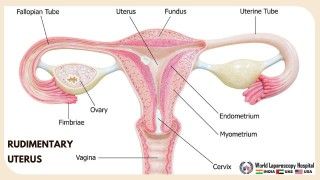
Laparoscopic Sigmoidectomy with Total Mesorectal Excision (TME) represents one of the most advanced and technically demanding procedures in minimally invasive colorectal surgery. At World Laparoscopy Hospital (WLH), this procedure is performed with precision, adhering to the highest standards of oncologic safety and minimally invasive excellence. Under the expert guidance of Dr. R. K. Mishra, surgeons are trained to perform this operation step by step, mastering both anatomical understanding and advanced laparoscopic techniques. Introduction Sigmoidectomy with TME is primarily indicated for patients with sigmoid colon or upper rectal cancer, complicated diverticulitis, or other localized diseases requiring segmental resection. The laparoscopic approach at WLH offers patients faster recovery, minimal pain, and reduced postoperative morbidity, while maintaining oncologic integrity through precise dissection of the mesocolon and mesorectum. Step 1: Patient Positioning and Port Placement The patient is placed in the modified lithotomy position with steep Trendelenburg and right tilt. The surgeon stands on the right side, the assistant on the left, and the monitor is positioned near the patient’s left foot. A five-port technique is typically used: Umbilical port for the camera (10 mm) Left and right lower quadrant ports for working instruments Additional ports for retraction and assistance Pneumoperitoneum is established, and the entire abdomen is explored to rule out metastasis or unexpected pathology. Step 2: Identification and Mobilization of the Sigmoid Colon The sigmoid colon is identified and elevated. The lateral peritoneal attachments (white line of Toldt) are incised using an energy device such as the Harmonic scalpel or Ligasure. This medial-to-lateral or lateral-to-medial dissection exposes the retroperitoneal plane, carefully protecting the ureter and gonadal vessels. Step 3: Vascular Control – Inferior Mesenteric Vessel Dissection The next step involves the dissection around the inferior mesenteric artery (IMA) and inferior mesenteric vein (IMV): The peritoneum is incised just below the sacral promontory. The IMA is skeletonized and divided close to its origin using hem-o-lok clips or a vascular stapler to ensure adequate lymphadenectomy. The IMV is divided near the ligament of Treitz to allow tension-free mobilization of the colon. This step ensures a clear and bloodless operative field for subsequent mobilization. Step 4: Total Mesorectal Excision (TME) TME is the cornerstone of oncologic rectal surgery. The dissection proceeds in the avascular areolar plane between the visceral and parietal pelvic fascia. Using sharp dissection and gentle traction, the mesorectal envelope is separated intact, preserving the autonomic nerves to avoid postoperative dysfunction. The posterior, lateral, and anterior planes are dissected systematically until the levator ani is reached. The rectum is divided at the predetermined level using an endoscopic linear stapler. This precise dissection minimizes local recurrence and ensures adequate margins. Step 5: Specimen Extraction and Anastomosis Once the sigmoid colon and rectum are mobilized: The specimen is retrieved either through a Pfannenstiel incision or a small protected extraction site. The proximal colon is prepared for anastomosis by ensuring adequate perfusion. A circular stapled colorectal anastomosis is performed under direct visualization, ensuring a tension-free, leak-proof join. The anastomosis is tested with air insufflation to confirm integrity. Step 6: Hemostasis, Irrigation, and Closure After meticulous hemostasis, the pelvis is irrigated with warm saline. A pelvic drain may be placed near the anastomosis if required. All ports are removed under direct vision, and the fascial defects at the larger port sites are securely closed. Postoperative Care Patients at WLH benefit from enhanced recovery protocols (ERAS): Early ambulation within 6 hours Oral fluids within 12–24 hours Minimal opioid analgesia Early discharge within 3–5 days post-surgery Continuous monitoring ensures the early detection of complications such as anastomotic leak or ileus. Conclusion Laparoscopic Sigmoidectomy with TME at World Laparoscopy Hospital exemplifies the perfect blend of oncologic safety, minimal invasiveness, and surgical precision. The procedure, when performed using the standardized step-by-step technique taught at WLH, offers excellent clinical outcomes, reduced hospital stay, and superior patient satisfaction. Through structured training, simulation, and live surgical exposure, WLH continues to shape the future of minimally invasive colorectal surgery, empowering surgeons worldwide with the skills and confidence to perform complex laparoscopic resections with excellence.
Similar Videos